Health CO-OPs of the Affordable Care Act
Promise and Peril at the 5-Year Mark
Allan M. Joseph, BA; Eli Y. Adashi, MD, MS - Warren Alpert Medical School, Brown University, Providence, Rhode Island
JAMA. Published online January 29, 2015.
In the early stages of drafting what would become the Affordable
Care Act (ACA), the notion of including a federal health insurance issuer in the
online marketplaces engendered an intense debate.1
Advocated with a goal of promoting choice and competition, the so-called public
option was to focus on the individual and small business markets.1 But it was not to be. Opposed by the health
insurance industry, characterized as a ggovernment takeoverh of health care, and
weighed down by concerns about a national single-payer health insurance system,
the public option proved unpassable.1 In its stead emerged the far less expansive if
politically palatable Consumer Operated and Oriented Plan (CO-OP)
program.2 The
nongovernmental, state-delimited CO-OP program was to gfoster the creation of
qualified nonprofit health insurance issuers to offer qualified health plans in
the individual and small group markets.h3
However, the CO-OPs (health insurance providers) should not be confused with
accountable care organizations (coordinated health care providers). In this
Viewpoint, we review the central tenets of the CO-OP program, assess its current
state of implementation, and describe its future
challenges.
As per statute, the state-chartered and -licensed CO-OPs
(freestanding distinct health insurance issuers) were to constitute private,
tax-exempt, consumer-operated and governed health insurance cooperatives.2 Modeled on member corporations
in the agricultural, utility, and financial sectors, the exchange-certified
CO-OPs were to issue at least two-thirds of all policies with the individual or
small-group markets in mind.3 Among the qualified health plans offered, at
least 1 was to feature gsilverh and ggoldh benefit packages whether on or off
the federal or state exchanges (government-run marketplaces of health insurance
plans).3 Encouraged to
operate statewide, CO-OPs were to establish integrated care models, develop
innovative (cost-saving) pay models, advance novel benefit designs, cultivate a
strong consumer focus, and incentivize wellness promotion.3 In particular, CO-OPs were to reinvest most net
earnings with the best interest of their membership in mind. Examples include
lowering premiums, expanding benefits, and improving quality.3 Low overhead costs were to be advanced by
reliance on private purchasing councils, preferred vendors, and grassroots
marketing efforts.3
It was the hope and expectation of the framers of the CO-OP
construct gthat there is sufficient funding to establish at least one qualified
nonprofit health insurance issuer in each State.h3
With this objective in mind, the CO-OP program was to be launched with 5-year
start-up and 15-year solvency low interest loans issued by the Centers for
Medicare & Medicaid Services.3 However, 3 sequentially enacted statutes later,
the ACA-proscribed budget of $6 billion has been reduced to $2.1 billion,
thereby all but eliminating the prospect of a nationwide CO-OP program.1,2
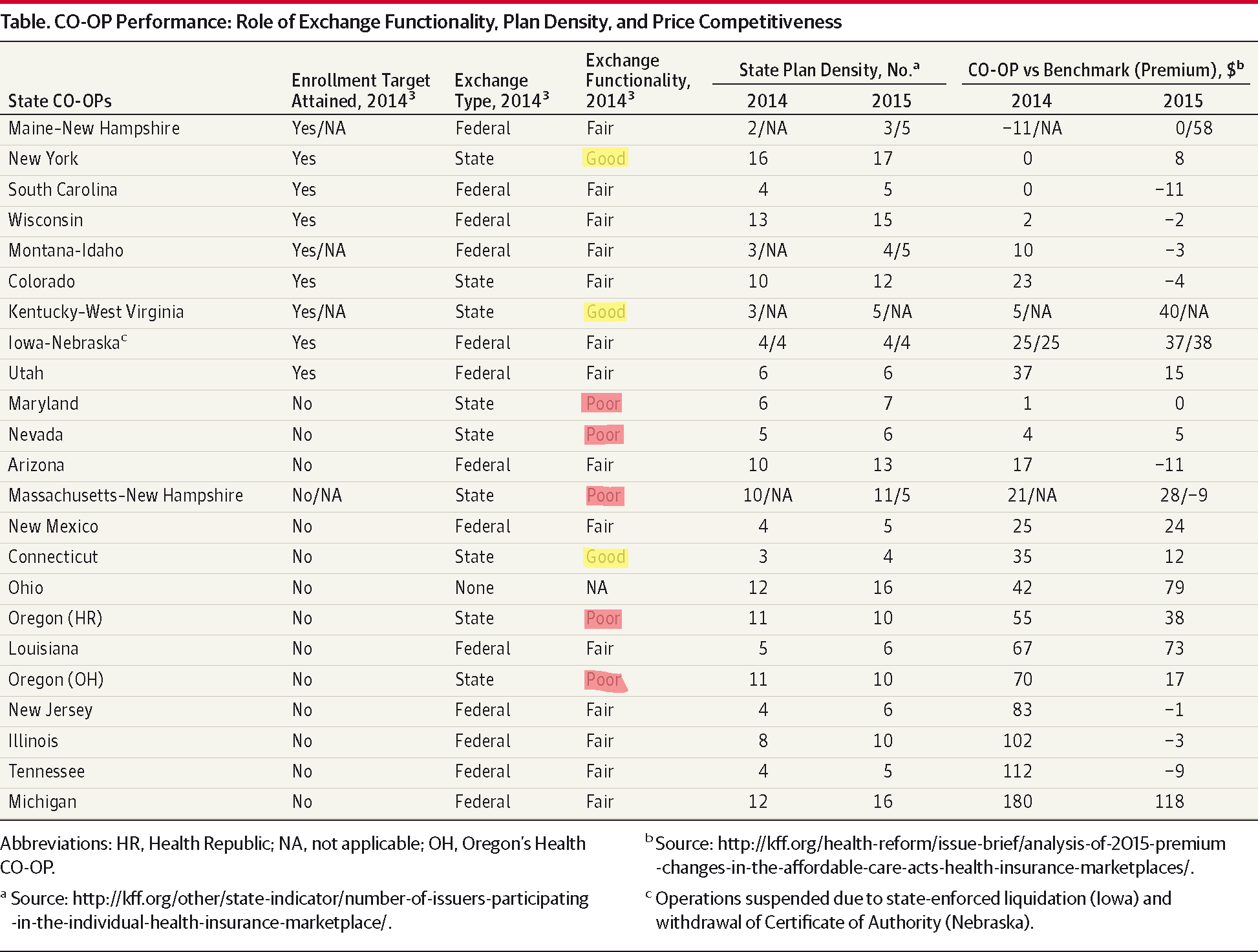
In the aftermath, a total of 23 state-based (private, not-for-profit) CO-OPs
have emerged.1,2 More recently, the national
complement of CO-OPs expanded to include New Hampshire, West Virginia, and Idaho
(Table) by way of newly launched
bi-state tandems (ie, CO-OPs serving 2 adjacent states, such as Kentucky–West
Virginia, Massachusetts–New Hampshire, and Montana–Idaho). In so doing, the
Centers for Medicare & Medicaid Services extended the reach of the CO-OP
program to a total of 26 states (Table) comprising an estimated 45% of the US
population.
gå}
By the end of the first ACA open-enrollment period (March 31,
2014), the 23 operational CO-OPs enrolled approximately 460 000 members, or 80%
of the total projected.4
However, the state enrollment records proved highly variable.4 Although 60% of the CO-OPs failed to reach
enrollment targets by wide margins, 40% either met or substantially exceeded
projected enrollment goals.4 The CO-OPs based in New York, Iowa-Nebraska, and
South Carolina alone accounted for more than half of all enrollees.4 What is more, CO-OPs based in
Kentucky and Maine dominated their online marketplaces, capturing 75% and 80% of
the market, respectively.
Viewed in hindsight, the 2014 enrollment record of a given CO-OP
appeared to depend on local determinants such as exchange functionality and
price competitiveness (Table). State
plan densities (ie, number of health insurance plans per state) appeared to have
played a more limited role. Overall, it appears that the CO-OPs have injected
welcome measures of choice and competition into the health insurance
marketplace. First, the CO-OPs introduced more products than any other new
entrant.5 Second, the
CO-OPs offered 37% of the lowest-priced plans in their home states.5 Third, premium rates were 9%
lower in states featuring a CO-OP as compared with states without one.5 More recent analysis suggests
that the CO-OPs have further increased their competitiveness on entry (November
15, 2014) into the second open-enrollment period. Relative to 2014, the premiums
of 10 rather than 3 CO-OPs are at or below the subsidy-determining benchmark
plan (gsecond-cheapest silver premiumh). However, increased plan densities in
virtually all states may pose an increasingly important challenge to the
CO-OPs.
Having crossed the start-up chasm with time to spare to loan
repayment (a 15-year horizon), the CO-OPs now face the imperative of growth to a
critical size compatible with sustainable ongoing operations. This requirement
is readily inferred from the experience of surviving legacy health CO-OPs (eg,
Group Health Cooperative of Puget Sound), some of which have in excess of
600 000 members.6 Absent
such economies of scale, access to new capital, or both, the newly established
CO-OPs may be unable to maintain liquidity, disperse risk, lower premiums,
exercise leverage, and establish branded statewide integrated care models.
Moreover, CO-OPs gtoo small to thriveh may default on their loans. Viewed in
this light, the road ahead is clear in calling for aggressive recruitment of
enrollees through competitive pricing and product diversification.7 Far less clarity exists with respect to the
possibility of adverse future legislative actions. At the very least, the CO-OPs
will remain under scrutiny by the House Committee on Oversight and Government
Reform, which has launched an investigation of the CO-OPs to examine the
gObamacare loan Guarantee Gambleh as a case study of gpolitical influence
peddlingh and gtaxpayer dollars wasted.h
At this time, the future of the existing CO-OP program remains
promising if uncertain. According to this view, some CO-OPs may falter. The
recent default of CoOpportunity Health, the CO-OP serving the states of Iowa and
Nebraska, is supportive of this outlook.8
Other CO-OPs may experience a significant growth spurt replete with the related
attendant benefits. The latter outcome hinges on the appeal of the CO-OP
construct, functional online exchanges, and priced-to-compete multiyear
products.7 Growth by way
of entry into the mid-size and large group markets must also be
considered.7 In the final
analysis, the CO-OPs will have to prove their effectiveness and value in the
marketplace. Only time will tell if the gCO-OP optionh—rising as it were from
the ashes of the public option—will in effect constitute a worthy successor to
its much-maligned forebear.
Corresponding Author: Eli Y.
Adashi, MD, MS, Warren Alpert Medical School, Brown University, 101 Dudley St,
Providence, RI 02905. (eli_adashi@brown.edu).
Published Online: January 29,
2015. doi:10.1001/jama.2015.501.
Conflict of Interest
Disclosures: The authors have completed and submitted the ICMJE Form
for Disclosure of Potential Conflicts of Interest and none were reported.
Funding/Support: Mr Joseph is
supported by a Summer Research Assistantship (SRA) from the Warren Alpert
Medical School, Brown University.